| Original Article Online Publishing Date: | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Sudan J Paed. 2023; 23(1): 74-81 SUDANESE JOURNAL OF PAEDIATRICS 2023; Vol 23, Issue No. 1 ORIGINAL ARTICLE Patterns and management outcome of paediatrics burn in a general surgical department: experience from a secondary referral hospitalMohammed Yousof Bakhiet (1,2), Mohammedbabalrahma Bashier Ahmed Koko (1), Mohamed Daffalla-Awadalla Gismalla (2,3), Sami Mahmoud Assil (4), Ahmed A. Bagit (5)(1) Department of Surgery, Faculty of Medicine, Kordofan University, Elobied, Sudan. (2) Department of Surgery, Faculty of Medicine, Albaha University, Albaha, Saudi Arabia. (3) Department of Surgery, Faculty of Medicine, University of Gezira, Medani, Sudan. (4) Department of Preventive Medicine, Tabuk Health Affairs, Saudi Arabia. (5) Temerty Faculty of Medicine, University of Toronto, Toronto, Ontario, Canada. Correspondence to: Mohammed Yousof Bakhiet Associate professor of Plastic Surgery, Department of Surgery, Faculty of Medicine, Kordofan University, Elobeid, Sudan. Email: bakhietmoh [at] yahoo.com Received: 20 October 2020 | Accepted: 28 March 2023 How to cite this article: Bakhiet MY, Koko MBA, Gismalla MD, Assil SM, Bagit AA. Patterns and management outcome of paediatrics burn in a general surgical department: experience from a secondary referral hospital. Sudan J Paediatr. 2023;23(1):74–81. https://doi.org/10.24911/SJP.106-1603179359 © 2023 SUDANESE JOURNAL OF PAEDIATRICS
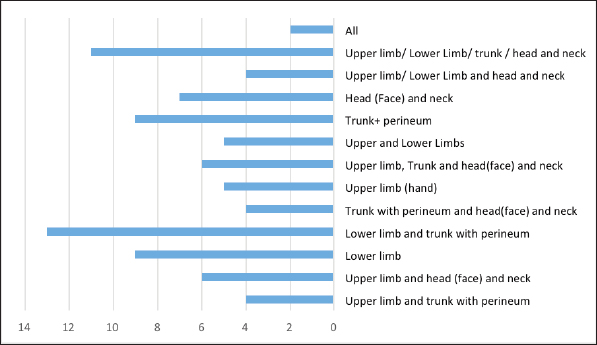
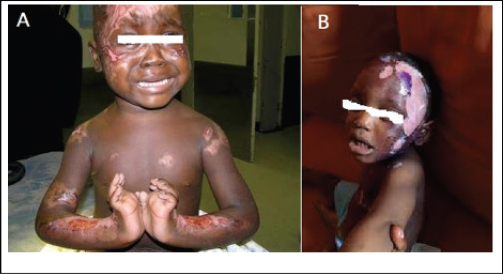
ABSTRACTBurns are considered the fourth most common type of traumatic injury worldwide with significant morbidity and mortality. The aim of this study is to disclose the incidence, etiological factors, treatment and outcome of paediatric burns in Sudan. This is a retrospective hospital-based study, conducted during 2016–2019. Patients who presented with burn injuries and managed in the hospital were included in the study. Flowchart sheets were used to collect the data. Then, it was entered and analysed using Statistical Package for the Social Sciences version 21 statistical software (IBM Corporation, Chicago, IL). The total number of patients who fulfill our criteria is 85 with a median age of 4 years (7 months–15 years). Sixty-five percent of them were under 5 years with male predominance (55%). Most patients’ burns occurred at home. The median percentage of burn is 18% (2%–90%) which is caused by scalding burn among 55.3% followed by the flame burn in 41.2% of patients. Regarding fluid management, 60% received fluid. Open dressing for burn wounds was done for 75% and close dressing among 15% of patients. More than 80% of the patients in this study were treated and discharged in a good condition while the mortality was 5.9%. This study showed the significant burden of paediatric burns management on general surgery units in a referral hospital. Therefore, equipping the hospital and founding these specialities will decrease this load and will improve the outcome. Keywords:Burn; Burn in paediatrics; Management outcome; Developing countries. INTRODUCTIONBurns signify one of the most disturbing physical and psychological injuries [1]. WHO reported that about 11 million victims of burn injuries occur worldwide annually [2]. Burns represent one of the most common causes of mortality and morbidity worldwide; the mortality rate is estimated to be more than 265,000 deaths worldwide. Despite an improvement in burn-associated surgical and medical care, there is still high mortality among patients who sustain burn injuries, especially in developing countries [3,4]. In Africa, paediatric burns are responsible for the largest number of hospital admissions with an estimated 18,000–30,000 deaths annually in sub-Saharan Africa [5]. Being ranked as the fourth most common type of trauma worldwide, burn injuries in the East Mediterranean Region, including Sudan, still remain a significant public health matter, with children being the most affected age group of patients [6]. Among many consequences of burns, physical disfiguring and social stigma is considered leading causes of decreasing one’s productivity [6,7]. Burns during childhood may result in long-term disability and also lead to deterioration in mental well-being and quality of life of families [8]. With a limited ability to react quickly and appropriately in hazardous conditions, children are at great risk of burns injuries [9]. In Sudan, the real situation of paediatric burns is not well known due to the lack of published reports documenting this problem. This study aims to report on the incidence, etiological factors, treatment and outcome of paediatric burns treated by a general surgeon in a secondary referral (not burn or paediatrics specialised hospital) in Sudan. MATERIALS AND METHODSStudy designThis is a retrospective hospital-based study, conducted in Elobeid Teaching Hospital, Elobeid, Sudan during 2016–2019. Study areaElobeid Teaching Hospital is a referral hospital in Kordofan State. Patients with emergency conditions, trauma and burns were received in the emergency departments. Burn cases were attended by a general surgical team who was covering the duty and initial treatment given to them. There are four general surgical units; each unit is headed by a consultant of general surgery. The hospital is comprised of an Accident and Emergency Department, Radiology Department, Laboratory Center with a blood bank, Surgical Specialty Department, Medical Specialty Department, as well as an operation complex with an Intensive Care Department. Inclusion and exclusion criteriaWe included all children who presented to the hospital with burns, during the study period and received treatment in the hospital. Patients aged more than 15 years were excluded from the study population. Initial assessment and interventionAny patient who presented to the emergency department was assessed by the team, including vital signs and surface area. All patients were managed by a local protocol followed by all units. Fluid replacement follows Parkland’s formula for any child with burns of more than 10% of body surface area. Ringer lactate has been used as the main type of fluid for resuscitation. Antibiotics were given if there is a sign of infection. A high-protein diet was used. Further managementAccording to the degree of burn wound care was established. For partial thickness dry dressing with open methods was done. For any deep thickness or nonresponding open methods, the closed dressing was used after a clean aseptic dressing. Any debridement was done under general anesthesia. A skin graft was used in some selective cases. Data collection and analysisFlowchart sheets were used to collect the baseline characteristics of the patients. Age, sex, residence and causes of burn were recorded. Further patients’ assessments regarding the surface area, fluid therapy, wound care and the outcome were determined. Types of operation and intervention were determined based on each individual case. The data collected were entered and analysed using Statistical Package for the Social Sciences version 21 statistical software (IBM Corporation, Chicago, IL). Results were tabulated and presented as frequencies and percentages, accordingly. For each test, p < 0.05 was considered statistically significant (95% CI). RESULTSThe total number of patients who fulfill our criteria is 85. The median age of the patients was 4 years ranging between 7 months and 15 years. Thirty-two percent of them were under 2 years and 65% of them were under 5 years. Males were predominant (47, 55%). Sixty percent of them are residents in Elobeid city while the others are residents outside the city. Two thirds of the patients (62%) presented to the hospital in the first 2 hours. The educational level of a child’s guardian was primary school (37%) and secondary school in 31%, while the others are not educated at all. Most patient burns occurred at home. Among 87% of patients. The other detailed patients’ characters are shown in Table 1. The median percentage of burn is 18% ranging from 2% to 95%. The commonest cause of the burn is scalding burn among 55.3% followed by flame burn in 41.2% of patients. Superficial burn and superficial partial thickness occurred among 52.9% and 24.7%, respectively. Deep partial thickness burn occurred in 12.9% and the rest was full thickness burn. As burns commonly affect multiple parts of the body, the combination of the lower limb, trunk, and perineum was the most commonly affected site in our cases. The detailed site-affected burn is shown in Figure 1. Figure 2 shows an example of different body sites affected by burns. Regarding fluid management, 60% received fluid during the initial management. The types of wound care used were open dressing in 75%and closed dressing at 15%. Nine percent of the cases needed plastic surgery intervention to cover their wound using skin grafts. More than 80% of the patients in this study were treated and discharged in a good condition. The mortality rate was 5.9%. The other patient clinical assessment, management, and outcome assessment are shown in Table 2. Table 1. Patient characteristics.
DISCUSSIONThis study was conducted in Elobeid Teaching Hospital which is the main referral hospital in the state where the surgical services were mainly carried out by general surgery units. There are no specialised paediatric surgery or plastic surgery units or burn unit. No one of our patients in this study had physiotherapy since the hospital has no specialised rehabilitation section. Therefore, the management of burn cases represents a great burden to general surgery units. The situation makes the management of burn cases a real challenge to have a good outcome. Nearly 50% of burn injuries affect the paediatric age group, with children less than 5 years accounting for 17% of all cases [6]. The total number of patients reviewed in this study was 85 patients which represents about two third of burn cases admitted to the hospital during the study period.
Figure 1. Anatomical site of burn among patients in the study.
Figure 2. Burns in different sites. Table 2. Patient clinical assessment management and outcome.
The dominating age group in our recorded data was below 5 years which conforms with the study done by Al Shareef Mohammad et al. [10] in a specialised paediatric center in Sudan as well as reports from other national and international data [11–13]. Most studies reported that males have a higher tendency to sustain burn injuries (male-to-female ratio of 1.2–1) [14]. Like other previously published national and international data [3,10,12–20] burns occur predominantly in males than females in our study. Interestingly, the time of presentation to the hospital following burn injury was in the first 2 hours in more than two-thirds of patients. This goes with the finding that most of the patients reside in Elobied city (60%) which in turn facilitates their arrival at the hospital. However, results from a study done in Sudan showed 55% of cases came from outside the city [10]. The absence of close supervision, alertness, and knowledge regarding the causes of burns is considered to directly affect children’s exposure to burns. The parent’s education regarding the safety measure taken at the house should be improved [19]. Using a high stand for and keeping boiling water away from their children could decrease the incidence of burns [13,16]. The presence of parents in the house does not prevent the occurrence of burn since our data showed that the site of burn is at home in more than 70% of cases. The mother’s level of education is primary and illiteracy in more than 68% of cases could indicate the dominance of burns among young children in our study. The commonest causes of burns in sub-Sahara Africa are scald (59%) followed by flame 33%. However, in Western Africa, the two causes have a similar ratio [14]. In our present study, the common cause of burn was scald burn in most of the cases. These results are in accordance with published literature in Sudan and other regional countries [9,10,12,14,16,20,21]. We have three cases of electrical burn which represent 3.5% of all cases which is considered to be higher than in this age as shown by many different studies [8,9,22]. However local reports showed the same percentage. Published data reported that the majority of paediatric patients have less than 20% of total body surface area (TBSA) burned [13], and our data are consistent with this literature, where the median percentage of burn is 18% [19]. The combined lower limb, trunk and perineum represents the common body sites affected by the burn in our data which conform with other published report from another study done in Sudan [10] and this could be explained by expel of hot fluid all over the body during the mechanism of the burning process. The depth of burns in our data is mainly superficial and superficial partial thickness and this is expected since the main cause of burn was scald. These findings were similar to reports of national and international reports [10,12,15,19]. Management of burn cases in sub of sub-Saharan Africa represents a real challenge to the governments in the presence of other infectious diseases like malaria [14]. Most of these countries have no formal protocol for the management of burns generally [14]. In Sudan, the situation is similar to the neighboring countries. In our series, the work of burn management is taken by the general surgery units in the hospital where they adopt a local protocol. This protocol consists mainly of early fluid resuscitation and wound care with debridement if needed and limited wound cover in the form of skin grafting in selected cases and according to their hospital setting. The amount of fluid is given according to the Parkland formula in the form of ringer lactate. More than half of the patients received fluid in their admission because of burns between 15% and 20% TBSA. The open method for wound dressing is used for wound treatment in more than three-quarters of cases which were proven successful and cost-effective in our setting. Studies done in Khartoum used the same method [10]. Burns injuries are the main reason for morbidity and mortality across sub-Saharan Africa [14]. In some low-income countries like Nepal, the mortality reached 50% to a burn size of 30% TBSA [23]. The management of burns in Elobied Teaching Hospital overall has a satisfactory outcome where there are no plastic surgery services as well as acting paediatric surgery unit. More than 80% of the patients recovered completely and 7% of them were referred to a plastic surgery center for further management. The mortality rate in our series is 5.9%, which was significantly affected by the mean percentage of TBSA. It is considered to be high if it is compared to other local reports published in specialised paediatric surgery centers in Sudan [10]. However, if we analysed our hospital setting, it would be reasonable and accepted, especially since the services were carried out by a general surgeon and no expertised plastic or paediatric surgery acting units. The actual credit goes to their valuable effort to have this outcome. CONCLUSIONThis study showed the significant burden of paediatric burns management on general surgery units in a referral hospital. So equipping the hospital and founding these specialities will decrease this load and will improve the outcome. Furthermore, establishing a national burn center will be beneficial in this context. CONFLICT OF INTERESTThe authors declare that they have no conflicts of interest. FUNDINGNone. ETHICAL APPROVALEthics committee approval was received for this study from the Administration Department of Elobeid Teaching Hospital. Written informed consent was obtained from parents of children included in the study. REFERENCES
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| How to Cite this Article |
| Pubmed Style Bakhiet MY, Koko MBA, Gismalla MD, Assil SM, Bagit AA. Patterns and management outcome of paediatrics burn in a general surgical department: experience from a secondary referral hospital. Sudan J Paed. 2023; 23(1): 74-81. doi:10.24911/SJP.106-1603179359 Web Style Bakhiet MY, Koko MBA, Gismalla MD, Assil SM, Bagit AA. Patterns and management outcome of paediatrics burn in a general surgical department: experience from a secondary referral hospital. https://sudanjp.com//?mno=17059 [Access: May 08, 2024]. doi:10.24911/SJP.106-1603179359 AMA (American Medical Association) Style Bakhiet MY, Koko MBA, Gismalla MD, Assil SM, Bagit AA. Patterns and management outcome of paediatrics burn in a general surgical department: experience from a secondary referral hospital. Sudan J Paed. 2023; 23(1): 74-81. doi:10.24911/SJP.106-1603179359 Vancouver/ICMJE Style Bakhiet MY, Koko MBA, Gismalla MD, Assil SM, Bagit AA. Patterns and management outcome of paediatrics burn in a general surgical department: experience from a secondary referral hospital. Sudan J Paed. (2023), [cited May 08, 2024]; 23(1): 74-81. doi:10.24911/SJP.106-1603179359 Harvard Style Bakhiet, M. Y., Koko, . M. B. A., Gismalla, . M. D., Assil, . S. M. & Bagit, . A. A. (2023) Patterns and management outcome of paediatrics burn in a general surgical department: experience from a secondary referral hospital. Sudan J Paed, 23 (1), 74-81. doi:10.24911/SJP.106-1603179359 Turabian Style Bakhiet, Mohammed Yousof, Mohammedbabalrahma Bashier Ahmed Koko, Mohamed Daffalla-Awadalla Gismalla, Sami Mahmoud Assil, and Ahmed A. Bagit. 2023. Patterns and management outcome of paediatrics burn in a general surgical department: experience from a secondary referral hospital. Sudanese Journal of Paediatrics, 23 (1), 74-81. doi:10.24911/SJP.106-1603179359 Chicago Style Bakhiet, Mohammed Yousof, Mohammedbabalrahma Bashier Ahmed Koko, Mohamed Daffalla-Awadalla Gismalla, Sami Mahmoud Assil, and Ahmed A. Bagit. "Patterns and management outcome of paediatrics burn in a general surgical department: experience from a secondary referral hospital." Sudanese Journal of Paediatrics 23 (2023), 74-81. doi:10.24911/SJP.106-1603179359 MLA (The Modern Language Association) Style Bakhiet, Mohammed Yousof, Mohammedbabalrahma Bashier Ahmed Koko, Mohamed Daffalla-Awadalla Gismalla, Sami Mahmoud Assil, and Ahmed A. Bagit. "Patterns and management outcome of paediatrics burn in a general surgical department: experience from a secondary referral hospital." Sudanese Journal of Paediatrics 23.1 (2023), 74-81. Print. doi:10.24911/SJP.106-1603179359 APA (American Psychological Association) Style Bakhiet, M. Y., Koko, . M. B. A., Gismalla, . M. D., Assil, . S. M. & Bagit, . A. A. (2023) Patterns and management outcome of paediatrics burn in a general surgical department: experience from a secondary referral hospital. Sudanese Journal of Paediatrics, 23 (1), 74-81. doi:10.24911/SJP.106-1603179359 |
Nagwa Salih, Ishag Eisa, Daresalam Ishag, Intisar Ibrahim, Sulafa Ali
Sudan J Paed. 2018; 18(1): 24-27
» Abstract » doi: 10.24911/SJP.2018.1.4
Siba Prosad Paul, Emily Natasha Kirkham, Katherine Amy Hawton, Paul Anthony Mannix
Sudan J Paed. 2018; 18(2): 5-14
» Abstract » doi: 10.24911/SJP.106-1519511375
Inaam Noureldyme Mohammed, Soad Abdalaziz Suliman, Maha A Elseed, Ahlam Abdalrhman Hamed, Mohamed Osman Babiker, Shaimaa Osman Taha
Sudan J Paed. 2018; 18(1): 48-56
» Abstract » doi: 10.24911/SJP.2018.1.7
Adnan Mahmmood Usmani; Sultan Ayoub Meo
Sudan J Paed. 2011; 11(1): 6-7
» Abstract
Mustafa Abdalla M. Salih, Mohammed Osman Swar
Sudan J Paed. 2018; 18(1): 2-5
» Abstract » doi: 10.24911/SJP.2018.1.1
Amir Babiker, Afnan Alawi, Mohsen Al Atawi, Ibrahim Al Alwan
Sudan J Paed. 2020; 20(1): 13-19
» Abstract » doi: 10.24911/SJP.106-1587138942
Hafsa Raheel, Shabana Tharkar
Sudan J Paed. 2018; 18(1): 28-38
» Abstract » doi: 10.24911/SJP.2018.1.5
Anita Mehta, Arvind Kumar Rathi, Komal Prasad Kushwaha, Abhishek Singh
Sudan J Paed. 2018; 18(1): 39-47
» Abstract » doi: 10.24911/SJP.2018.1.6
Majid Alfadhel, Amir Babiker
Sudan J Paed. 2018; 18(1): 10-23
» Abstract » doi: 10.24911/SJP.2018.1.3
Bashir Abdrhman Bashir, Suhair Abdrahim Othman
Sudan J Paed. 2019; 19(2): 81-83
» Abstract » doi: 10.24911/SJP.106-1566075225
Amir Babiker, Mohammed Al Dubayee
Sudan J Paed. 2017; 17(2): 11-20
» Abstract » doi: 10.24911/SJP.2017.2.12
Cited : 8 times [Click to see citing articles]
Mustafa Abdalla M Salih; Satti Abdelrahim Satti
Sudan J Paed. 2011; 11(2): 4-5
» Abstract
Cited : 4 times [Click to see citing articles]
Hasan Awadalla Hashim, Eltigani Mohamed Ahmed Ali
Sudan J Paed. 2017; 17(2): 35-41
» Abstract » doi: 10.24911/SJP.2017.2.4
Cited : 4 times [Click to see citing articles]
Amir Babiker, Afnan Alawi, Mohsen Al Atawi, Ibrahim Al Alwan
Sudan J Paed. 2020; 20(1): 13-19
» Abstract » doi: 10.24911/SJP.106-1587138942
Cited : 4 times [Click to see citing articles]
Mutasim I. Khalil, Mustafa A. Salih, Ali A. Mustafa
Sudan J Paed. 2020; 20(1): 10-12
» Abstract » doi: 10.24911/SJP.1061585398078
Cited : 4 times [Click to see citing articles]